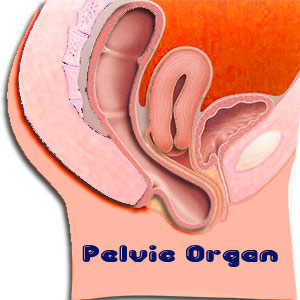
Pelvic Organ Prolapse
Prolapse is not uncommon. After childbirth, hysterectomy or menopause, some women develop pelvic organ prolapse. This happens when the muscles and ligaments supporting the pelvic organs weaken. The pelvic organ slips out of place, that is, prolapses, and such prolapses can worsen over a period of time.
Many physicians and gynecologists routinely screen patients for prolapse now, and a new surgical specialty urogynecology has developed to correct this problem. Statistics reveal that by age 80, more than 1 in every 10 women undergoes surgery for prolapse.
What is pelvic organ prolapse ?
This refers to the drop (prolapse) of your bladder from its normal spot in the lower abdomen and is pushed against the walls of the vagina. This happens when the muscles holding your pelvic organs weaken or get stretched from childbirth or after a surgery. The good news is that pelvic organ prolapse need not always get worse. In some women, it can get better with time.
More than one organ can prolapse at once and the organs involved in the pelvic prolapse include bladder, urethra, uterus, vagina, small bowel and rectum.
Types
There are different types of pelvic organ prolapse and they affect different parts of her vagina.
Cystocele and urethrocele occur when the bladder protrudes into the front wall of the vagina. The urethra presses into the front vaginal wall when a small defect - urethrocele - develops.
Rectocele is when the rectum bulges into the back of the vagina and sometimes this causes defecation.
Uterine prolapse occurs when the uterus drops down into the vagina.
The Baden-Walker System, a classification system standardizes the degree of descent of the anterior vaginal wall, cervix or vaginal apex and the posterior vaginal wall. The degree of prolapse is usually evaluated by Valsalva maneuver while the patient is placed in the lithotomy position (positioning of the patient's feet above or at the same level as the hips).
Degrees of Prolapse
| Stage I Prolapse | Descends halfway to the hymen | Stage II Prolapse | Descends to the hymen | Stage III Prolapse | Descends halfway past the hymen | Stage IV Prolapse | Descends to the maximum possible level |
Causes for prolapse
Pelvic organ prolapse is linked to various causes:
Strain during childbirth, when the pelvic organs tend to get weak and stretched. If they do not recover in course of time, they cannot support the pelvic organs.
You may have had a surgery to remove the uterus. This can sometimes leave other organs in the pelvis with lesser support.
Pelvic organ prolapse can result on account of repetitive straining; like those who are chronically constipated or those whose jobs entail heavy lifting. Pelvic organ prolapse can get worse if pressure is felt on the belly due to:
- Obesity
- Persistent Coughing
- Pelvic organ tumors.
Pelvic prolapse tends to be hereditary and older women are more likely to face this condition.
Symptoms
While those with mild prolapse exhibit no symptoms at all, there are others who experience considerable amount of symptoms including:
Pressure and pain: You could feel an overbearing pressure of the pelvis or leg fatigue or lower back pain.
Urinary symptoms: Urinary incontinence due to stress or an urgency to urinate a lot and sometimes difficulty in starting to urinate. Women suffering prolapse experience symptoms such as obstructive voiding, urinary hesitancy, intermittent flow and feeling of incomplete emptying of bladder.
Bowel symptoms: A rectocele can cause problems by forming a pocket just above the anal sphincter. Sometimes when stool become trapped, you may face pain, pressure and constipation.
Sexual problems: As vaginal tissues are irritated during a prolapse, pain during intercourse and psychological stress might be felt.
You may feel very full in the belly, as if something is falling out of the vagina and a pull or stretch in the groin area or pain in the lower back.
Treating prolapse
Decisions about your treatment will depend upon which pelvic organs have prolapsed and how bad the symptoms are. In case the symptoms are mild, then many of the symptoms can be avoided if healthy habits are adapted. Special exercises help to keep you stronger.
The doctor may recommend treating prolapse without surgery first. Whereas in some, the symptoms are so significant that they affect the quality of life and surgery becomes imperative.
Medications
As menopause results in lower estrogen levels, the muscles in your vagina tend to weaken. Estrogen therapy could strengthen the muscles. Before using estrogen, discuss your health issues with the doctor.
Physical therapy: This includes pelvic floor exercise using biofeedback to strengthen specific muscles of the pelvic floor. Biofeedback uses monitoring device with sensors that are placed in the vagina, rectum or on skin, and a computer shows whether you are using right muscles.
Surgery
The corrective surgical procedures to treat prolapse are SSLF (Sacrospinous ligament fixation) and ULS (Uterosacral ligament vaginal vault suspension).
- A surgery for posterior prolapse is done to secure the connectivity between the vagina and rectum to keep the rectum in its proper position. The excess tissue is removed.
- Anterior prolapse involves bladder and is called cystocele. The connective tissue between the bladder and vagina is restored to its proper position. In case of urinary incontinence, the doctor uses the bladder neck suspension or sling to support the urethra.
- Uterine prolapse is a surgery to remove the uterus to correct uterine prolapse.
- Small bowel and vaginal prolapse, sometimes called enterocele, is common among women who have had hysterectomy. The corrective surgery is performed through the vagina or abdomen. The surgeon uses ligaments that can support the uterus to correct the problem. In abdomen approach which is performed laproscopically or as an open procedure, the vagina gets attached to the tailbone at the base of the spine and small portions of synthetic mesh is used to support vaginal tissues. This is also called vaginal vault suspension. The tissue bulge is repaired by the prolapse surgery. In case, the bulge does not bother you, there is no need for surgery.
- Colpocleisis - the surgical closure of Vagina may be an easy and effective solution for elderly women who are not sexually active.
- Sacrospinous cervicocolpopexy - a surgical operation intended to restore support to the Uterus or Vaginal vault, performed on the Sacrospinous ligament ( called as sacrospinous fixation) with Uterine suspension might be suitable for women who are sexually active but would prefer to avoid hysterectomy.
Complications:
Possible complications of pelvic reconstructive surgery include:
- Infection of the urinary tract
- Temporary or permanent urinary incontinence
- Infection
- Bleeding
- Damage to the urinary tract, though rare, and this may require additional corrective surgery
- Chronic irritation or pain during intercourse.
- The risk or recurrence is highest for cystocele and lowest for rectocele.
Simple approach to treating prolapse
This can often be treated without surgery especially at the early stages when the prolapse is mild. A vaginal pessary devised from silicone can be inserted to support the vaginal walls. This device has to be removed and then inserted again every week.
Pelvic floor muscle training is a program that is customized to suit individual needs. This is done with the help of a physiotherapist, or continence nurse advisor.
Understand what caused your prolapse and make suitable lifestyle changes such as improving diet, fluid intake, exercising and losing weight. Become conscious of bowel and bladder habits and avoiding straining.
Top of the Page: Pelvic Organ Prolapse
Tags:#pelvic organ prolapsed #uterus prolapse #uterine prolapse

Enlarged Uterus
Bacterial Vaginosis
Yeast Infection
Irregular Menstrual Cycle
PMS - Menstruation
Dysmenorrhea
Hypomenorrhea
Mid Cycle Bleeding
Pelvic Organ Prolapse
Vaginal Atrophy
Cervix Cancer
Abnormal Pap Smear
Polycystic Ovarian Syndrome
Ovulation Pain
Uterine Prolapse
Fibroid Tumor
Menorrhagia
Endometriosis Symptom
Galactorrhea
Hysterectomy
Blocked Fallopian Tubes
Menopause and Weight Gain
Premature Menopause
Surgical Menopause
Other health topics in TargetWoman Women Health section:
General Women Health

Women Health Tips - Women Health - key to understanding your health ...
Cardiac Care
Women's Heart Attack Symptoms - Identify heart problems...
Skin Diseases
Stress Hives - Red itchy spots ...
Women Disorders
Endocrine Disorder - Play a key role in overall wellbeing ...
Women's Reproductive Health
Testosterone Cream for Women - Hormone replacement option ...
Pregnancy
Pregnancy - Regulate your lifestyle to accommodate the needs of pregnancy ...
Head and Face
Sinus Infection - Nearly 1 of every 7 Americans suffer from ....
Women and Bone Care
Slipped Disc - Prevent injury, reduce pain ...
Menstrual Disorders
Enlarged Uterus - Uterus larger than normal size ...
Female Urinary Problems
Bladder Problems in Women - Treatable and curable ...
Gastrointestinal Disorders
Causes of Stomach Ulcers - Burning feeling in the gut ...
Respiratory Disorders
Lung function Test - How well do you breathe ...
Sleep Management

Insomnia and Weight Gain - Sleep it off ...
Psychological Disorders in Women
Mood swings and women - Not going crazy ...
Supplements for Women
Women's Vitamins - Wellness needs...
Natural Remedies

Natural Diuretic - Flush out toxins ...
Alternative Therapy
Acupuncture Point - Feel the pins and needles ...
Top of the Page: Pelvic Organ Prolapse
Popularity Index: 100,935

