Ulcerative Colitis
Ulcerative colitis, Crohn's disease, rheumatoid arthritis, atherosclerosis, all these diseases have a common factor. All the four diseases can be traced to chronic inflammation. Of the four, ulcerative colitis closely mimics Crohn's disease. Symptoms are very similar and can often be confusing.
There are certain distinctive characteristics that clearly differentiate both. People with Crohn's disease have more sores around the anus than those with ulcerative colitis. To avoid confusion, learn more about ulcerative colitis. Check out the risk factors of developing ulcerative colitis, symptoms and treatment options. Find out why and how postponing a visit to medical expert can worsen the situation and complicate the condition.
Inflammatory bowel disease
Bowel function is an important function of the human body. Typically,
in healthy individuals, stool or feces is composed of water, dead and living
bacteria, fiber or undigested food, intestinal mucous and sloughed-off lining
of the gut. Also, feces are soft enough to pass comfortably. The activity part
of good digestion, if normal, can take place once or two times a day.
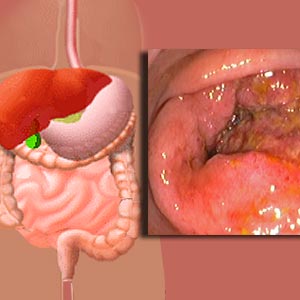
But for those with ulcerative colitis, bowel function is not normal. This is because the large intestine becomes inflamed and ulcers may develop. The inflammation starts in the last few inches of the large intestine. It is here the feces is stored before it leaves the body.
Ulcerative colitis symptoms
Symptoms of ulcerative colitis vary depending on the severity of inflammation and location of inflammation. The general symptoms are bloody diarrhea, rectal pain, urgency in moving bowels, loss of appetite, weight loss, fatigue and night sweats. Medical doctors classify ulcerative colitis based on severity of inflammation and location. There are specific symptoms for each type of classification.
Ulcerative proctitis: This is considered to be the mildest form of ulcerative colitis. The inflammation is limited to the rectum. Symptoms include rectal bleeding with or without rectal pain, a feeling of urgency or an inability to move bowels despite the urge to do so.
Proctosigmoiditis: In this form, both the rectum and the lower end of colon are affected. It can cause bloody diarrhea, abdominal cramps and pain.
Left-sided colitis: True to its name, the inflammation starts at the rectum and extends up the left colon. Symptoms include bloody diarrhea, abdominal cramps, weight loss and left-sided abdominal pain.
Pancolitis or universal colitis: It refers to inflammation affecting the entire colon. Symptoms include bloody diarrhea, abdominal pain and cramps, weight loss, fatigue, fever and night sweats.
Fulminant colitis: Not so common, this is a severe form of pancolitis. Symptoms include dehydration, severe abdominal pain, and protracted diarrhea with bleeding and even shock (a condition where body suffers from insufficient blood flow throughout body).
A unique feature of ulcerative colitis is that the affected individuals may have periods of time with no or some symptoms (called remission) and at times feel acutely sick (called relapse). But, in due course of time, the severity of the disease tends to remain the same. Individuals with milder conditions usually don't go on to develop more severe symptoms.
Ulcerative colitis is most likely to be associated with problems in other parts of the body. The affected individual may suffer from inflammation of the joints, eye problems and anemia due to blood loss.
Ulcerative colitis causes
Medical experts are still clueless regarding exact causes of ulcerative
colitis. To a certain extent, there is evidence which suggests that it is a
reaction of body's immune system response to a virus or bacteria by causing
inflammation in the intestinal wall. This evidence is yet to be proved scientifically.
Stress is totally ruled out as a causative factor. Likewise, certain foods or
food products cannot be primarily contributing but may set off symptoms.
Certain risk factors identified are:
Age: Problems can develop at any age. Yet, it is
most likely to develop between 15-30 years of age or sometimes in people aged
50-60.
Race and ethnicity: Caucasians and people of Jewish ancestry are considered to be at high risk of developing ulcerative colitis.
Heredity: Ulcerative colitis tends to run in families.
Gender: The chances of developing ulcerative colitis in the later part of life i.e. 50-60s are high for men than for women.
Ulcerative colitis
Postponing or watchful waiting may only add distress, increase
complications, sometimes turn life-threatening and worsen condition. It is best
to contact family medical doctor at the earliest. Never ignore periods of
recession. If the bowel movements continue to be persistently abnormal, contact
medical doctor immediately. Check out for persistent abdominal pain, blood in
stool, no respite from bouts of diarrhea in spite taking over-the-counter
medications and or fever lasting for a day or two.
Ulcerative colitis diagnosis
Certain question related to understanding patient's medical history will
be asked. This will be followed by a complete physical examination checking for signs such as paleness (caused
by anemia) and tenderness in the stomach (caused by inflammation). Certain special tests will then be
recommended.
Blood tests: Blood tests are conducted to check anemia and high white blood count. In case there is an elevated white blood cell count it reflects ongoing inflammation in the colon.
Stool examination: The stool sample is checked for blood which could mean intestine bleeding. In order to rule out bacterial or viral infection, stool specimens are collected and analyzed.
Colonoscopy or sigmoidoscopy: In order to confirm the diagnosis of ulcerative colitis or to determine the extent of inflammation inside the intestine, colonoscopy or sigmoidoscopy tests are recommended. The procedure is not painful but a sedative is administered to make patient feel relaxed. A long, flexible tube with a camera at the end called an endoscope will be inserted into the anus. The colon and rectum is checked. Inflammation, bleeding, or ulcers on the colon wall is checked. Sometimes, a sample tissue from the lining of the colon may be examined with a microscope.
Barium enema x-ray: The colon is filled with barium, a chalky white solution to facilitate a detailed view of the colon. The test is conducted to check any ulcers or other abnormalities.
Ulcerative colitis treatment
There is no cure for ulcerative colitis. Anti-inflammatory agents play a major role in controlling the
symptoms. If the diagnosis confirms the presence of ulcerative colitis, the patient is referred to a Gastroenterologist
to assess the severity of the condition and to decide further course of
treatment. The Gastroenterologist is likely to ask the patient questions such
as:
- How many times stools are passed in a day
- If stools are bloody
- If patient experiences symptoms of fever
- If patient is able to have control over bladder
- And about over-all well-being.
If the condition is severe, admission to hospital is advised. Otherwise, mild to moderate cases are treated on an out-patient basis. Medical professionals follow two types of treatment of ulcerative colitis.
- Managing active ulcerative colitis by treating the symptoms till it goes into remission
- Maintaining remission by using treatment to prevent the relapse or return of symptoms.
Managing active ulcerative colitis
Treatment options that don't involve surgery are the first choice.Aminosalicylates, steroids and
immunosuppressant are three types of medicines used to manage active ulcerative
colitis.
Aminosalicylates: Mostly used to treat mild to moderate ulcerative colitis, aminosalicylates help reduce inflammation. A medicine is also prescribed to relax the patient or relieve pain, diarrhea or infection. Aminosalicylates are available in various forms depending on the severity and extent of the condition. Doctors have the option of prescribing it in oral form as a tablet, a cream to be rubbed into the affected area or as a capsule which should be inserted into the rectum when it can dissolve or a fluid that is pumped into the colon.
Steroids : There are two reasons for steroids to be used. One, if ulcerative colitis is more severe and secondly if aminosalicylates are not effective enough. Steroids are similar to aminosalicylates but are stronger and powerful than aminosalicylates. Steroids are available in form of tablets, cream or suppository or enema. As long term use of oral steroids can cause serious side effects, it must be discontinued as soon as the colitis responds to treatment.
Immunosuppressant: In most cases, immunosuppressant is recommended if the on-going treatment is not effective enough, if steroids have to be withdrawn, to reduce possible side effects of medication. Immunosuppressant may also be used in combination with other medicines.
Maintaining remission
In order to maintain remission of symptoms, a regular dose of
aminosalicylates is prescribed. The symptoms are controlled from recurring. In
case the symptoms reoccur on a frequent basis, a regular dose of
immunosuppressant is prescribed. However, in case ulcerative colitis is
extensive, a lifelong maintenance therapy will be recommended.
Ulcerative colitis surgery
Most cases do not require a surgery. It is an option only when
ulcerative colitis does not respond to intensive medical treatment and the
condition adversely impacts patient's quality of life. Before any type of
surgery, doctors explain details such as:
- Why the surgery is done.
- The duration of the surgery.
- The duration of hospitalization.
- Procedures before, during and after surgery.
- The duration of rest at home post surgery.
- Extent of support required at home post surgery.
There are different types of surgery. Most common one is removal of colon and rectum. Removal of the colon is recommended when there is massive bleeding, severe illness, and rupture of the colon and if there is risk of cancer. Waste is rerouted from the colon so that it can pass waste products out of the body.
Another recent technique known as ilio-anal pouch may also be followed. It involves constructing an internal pouch inside the lower abdomen. Waste is collected in the pouch. The pouch is connected to the muscles surrounding the anus. It functions much like the colon.
Coping with ulcerative colitis
The pain, distress, physical discomfort associated with ulcerative
colitis can create great emotional stress for the patient. It can lead to
depression; make the person feel utterly frustrated, helpless and desperate for
support. The role of family is important. Here is information to help the individual.
- Diet is commonly overlooked and not give due importance. Find foods that contribute to
aggravating symptoms and those that help reduce flare-ups.
- Engaging in exercise that causes least discomfort can improve self-image. Talk to
doctor, learn exercises that can
help reduce stress, relieve depression and normalize bowel function.
- Check how hypnosis may reduce abdominal pain and bloating. A trained professional can
teach you how to enter a relaxed state.
- Find a support group. Talking with people about a common problem can be soothing and comforting.
It reduces anxiety, symptoms can aggravate if patients get overly anxious.
- Hospitals provide counseling. Enroll for hospital counseling or for counseling services
outside hospital. Venting out feelings and getting help to deal with emotional
and associated upheavals helps.
- Ensure medications are taken on time and never missed. During remission, medicines are
avoided or totally stopped. Explain the importance of completing prescribed
course.
Top of the Page: Ulcerative Colitis
Tags:#ulcerative colitis #ulcerative colitis pain #ulcerative colitis treatment #ulcerative colitis surgery #ulcerative colitis causes
Causes of Stomach Ulcers
Abdominal Hernia
Internal Body Cleansing
Ulcerative Colitis
Irritable Bowel Syndrome
Acid Reflux Syndrome
Belly Bloat
Inflammatory Bowel Disease
Groin Hernia in Woman
Carcinoid
Colonoscopy Procedure
Bariatric Surgery
Hemorrhoids
Colon Cleansing
Other health topics in TargetWoman Women Health section:
General Women Health

Women Health Tips - Women Health - key to understanding your health ...
Cardiac Care
Women's Heart Attack Symptoms - Identify heart problems...
Skin Diseases
Stress Hives - Red itchy spots ...
Women Disorders
Endocrine Disorder - Play a key role in overall wellbeing ...
Women's Reproductive Health
Testosterone Cream for Women - Hormone replacement option ...
Pregnancy
Pregnancy - Regulate your lifestyle to accommodate the needs of pregnancy ...
Head and Face
Sinus Infection - Nearly 1 of every 7 Americans suffer from ....
Women and Bone Care
Slipped Disc - Prevent injury, reduce pain ...
Menstrual Disorders
Enlarged Uterus - Uterus larger than normal size ...
Female Urinary Problems
Bladder Problems in Women - Treatable and curable ...
Gastrointestinal Disorders
Causes of Stomach Ulcers - Burning feeling in the gut ...
Respiratory Disorders
Lung function Test - How well do you breathe ...
Sleep Management

Insomnia and Weight Gain - Sleep it off ...
Psychological Disorders in Women
Mood swings and women - Not going crazy ...
Supplements for Women
Women's Vitamins - Wellness needs...
Natural Remedies

Natural Diuretic - Flush out toxins ...
Alternative Therapy
Acupuncture Point - Feel the pins and needles ...
Top of the Page: Ulcerative Colitis
Popularity Index: 101,066

